About Scleroderma
Scleroderma, or Systemic Sclerosis, is a chronic connective tissue dIsease generally classified as one of the autoimmune rheumatic diseases. The word “scleroderma” comes from two Greek words; “skleros” meaning hard and “derma” meaning skin.
Hardening of the skin is considered the hallmark of the disease. This hardening is caused by the overproduction of collagen which is laid down in the skin and internal organs resulting in scarring and reduced function of the affected organs.
Scleroderma is NOT contagious, infectious, cancerous or malignant.
Symptoms Scleroderma
The symptoms of Scleroderma vary significantly for each person, with the effects ranging from mild to life-threatening.
- Thickening of the skin causing a tight and shiny appearance
- Heartburn or Reflux
- Difficulty in swallowing
- Increased sensitivity to cold in the hands and feet (Raynaud’s Phenomenon)
- The appearance of tiny blood vessels on the skin (Telangiectasia)
- Difficulties in breathing or shortness of breath
What Does Scleroderma Affect?
The number of people who have Scleroderma in Australia varies from source to source, although it is widely accepted that this number is between 5000 and 10000. Overall female patients outnumber male patients by 4 to 1, with the onset of the disease generally being most prevalent between 25 and 55. There is no conclusive evidence to suggest that Scleroderma is hereditary.
What Causes Scleroderma?
The precise cause of Scleroderma is still unknown, however, research into the possible cause/s actively continues by medical and scientific communities all over the world.
Can Scleroderma be cured?
As the precise cause of Scleroderma has not yet been determined, there is currently no cure for the disease. Treatment consists of maintenance of the symptoms with the view to slowing disease progression and improvement in the quality of life for the patient.
Types of Scleroderma
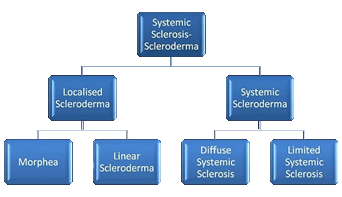
Localised Scleroderma
Localised Scleroderma affects the skin, related tissues and sometimes the muscle below. The internal organs are not involved and this form of the disease cannot progress into systemic sclerosis. Children are more likely to develop localised scleroderma than adults.
The two main types of localised scleroderma are Morphea and Linear scleroderma.
Systemic Sclerosis can be divided into two categories; limited and diffuse.
Limited Systemic Sclerosis
Limited Systemic Sclerosis tends to develop gradually over a number of years and is generally less severe than Diffuse Scleroderma. It is often referred to as CREST, an acronym for the following;
- Calcinosis - calcium deposits under the skin
- Raynaud's phenomenon - spasms in the small blood vessels of the hands and/or feet in response to cold or anxiety.
- Esophageal dysfunction - in the upper esophagus causing swallowing difficulties and in the lower esophagus causing chronic heartburn.
- Sclerodactyly - thickened skin on the fingers caused by excess collagen resulting in an inability to bend or straighten the fingers.
- Telangiectasia - small broken blood vessels on the surface of the skin.
Diffuse Systemic Sclerosis
In contrast to the limited form, Diffuse Systemic Sclerosis usually develops suddenly with a larger part of the body being affected. The damage to internal organs tends to be more severe with the long term outlook being the most serious of all the forms of this disease.